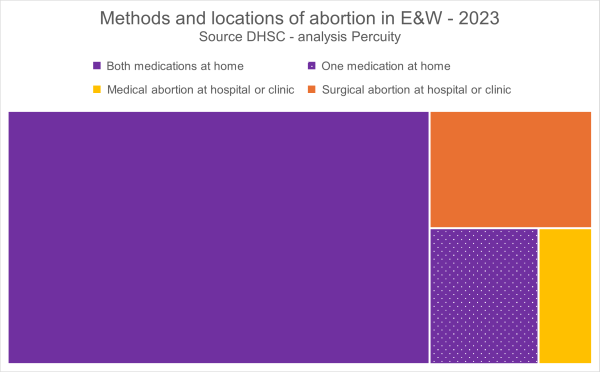
In recent years, across England and Wales, there has been a huge shift in how and where abortions are performed. Data published by the Department of Health and Social Care for 2023 show that five in every six abortions are now performed at home by the woman herself. Only five years prior to this, in... Continue Reading →
Is the DHSC counting prescriptions rather than abortions
Don’t panic, it's just an increase in prescriptions, not abortions. This has been the response from some, including in an article published by the Academy of Ideas, to the 30% increase in reported abortions in 2023 compared to 2021, as in the following quote: If a woman finds herself pregnant, and is considering what to... Continue Reading →
54,000 complications to medical abortion over the past five years – Baroness Sugg
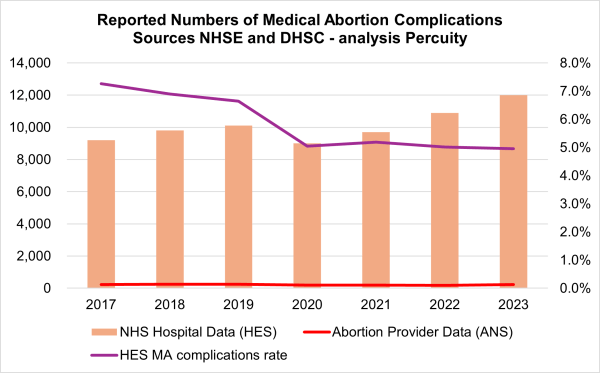
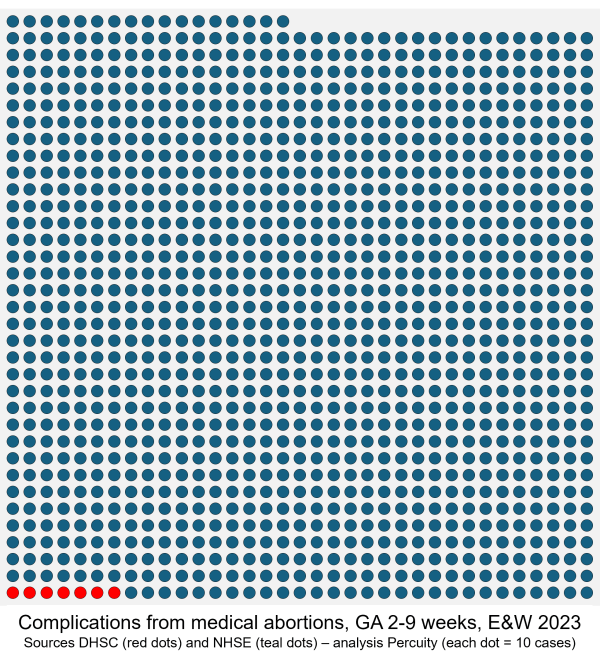
On 02 February, whilst speaking in defence of Clause 191 which will decriminalise abortion for women, Baroness Sugg confirmed: “There have been 54,000 complications to medical abortion over the past five years…” [i] This is the estimated total number of women admitted to an NHS hospital for treatment of complications arising from a medical abortion... Continue Reading →
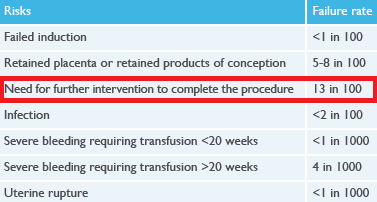
It is nothing like one in 17
Baroness Gerada was right, the figures from RCOG do not say that 1-in-17 women end up having complications from a medical termination, the number it states is actually more than twice that, 13% — 1-in-8 — nothing like one in 17. On 02 February 2026, the House of Lords met as a Committee to discuss... Continue Reading →
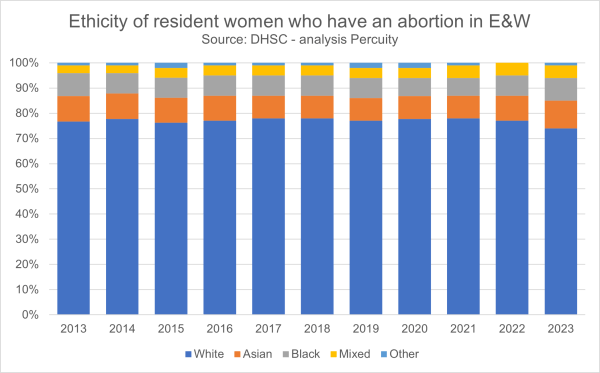
Are abortions disproportionately White?
Abortion numbers in England and Wales are highest among White women simply because they are the largest ethnic group. When adjusted for population size, White women do not have disproportionately high abortion rates. Their share of abortions broadly matches their share of women of reproductive age. It is worth noting though that White women have... Continue Reading →
Government fails to report 99% of early medical abortion complications
Analysis of abortion complications data published by the DHSC and by NHS England shows that the government continues to deliberately under-report, and that it has excluded more than 99% of complication treatments for early medical abortions, from its official 2023 statistics report. On 15 January 2026, the Department of Health and Social Care (DHSC) published... Continue Reading →
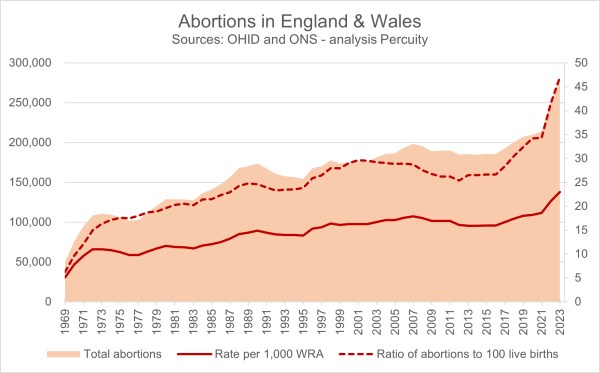
2023: an 11% increase in abortion across England and Wales
OHID: “There were 277,970 abortions for residents of England and Wales in 2023, the highest number since the Abortion Act was introduced and an increase of 11% compared with 2022.” [i] The government has just published the 2023 abortion statistics for England and Wales (15 January 2026). These were originally expected in June 2024 and... Continue Reading →
Five key insights
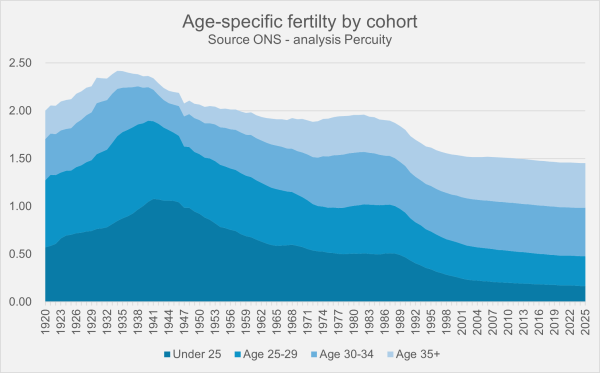
For every three conceptions in UK: one girl, one boy, one abortion. Birth rates have dropped so significantly that our natural population is projected to halve within two generations. Increasingly, young women are delaying motherhood; half remain childless by age 30. Women who are childless at 30 face a 50% chance of remaining childless by... Continue Reading →
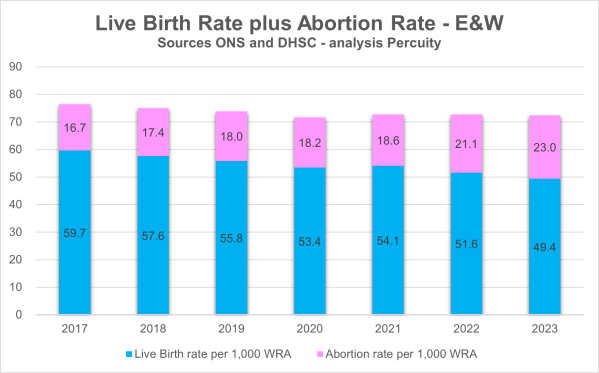
Ratio of abortions to live births
On 17 November 2025, Philip Pilkington, an economist and senior researcher at the Hungarian Institute of International Affairs, posted a thread on X in which he said “Britain is in a phase of self-euthanisation.” [i] He shared some data analysis, including mine,[ii] showing that in 2024 one-third of all viable pregnancies ended in abortion. He... Continue Reading →
It is not possible on the telephone to ensure a woman’s privacy, to ensure that she is not being coerced. Government stats show that, since 2020, 54,000 people have been admitted to hospital in England for complications from abortion pills. Last year alone, some 12,000—over 6% of women taking such medication—required hospital treatment. To safeguard... Continue Reading →
Abortion and childlessness
In the next two generations, our natural population is projected to halve, a decline driven largely by increasing childlessness. Current projections suggest that more than 25% of women reaching age 45 in the next 20 years, will do so without having children, and abortion plays a role in about half of these cases. Demographers have... Continue Reading →
Research organisation Percuity reported that, according to the NHS data, 1-in-17 women who had an abortion at home required hospital care for complications including incomplete abortions, infections, and excessive haemorrhages.
The Christian Institute
The Real Fertility Crisis: wanting, not just affording, children
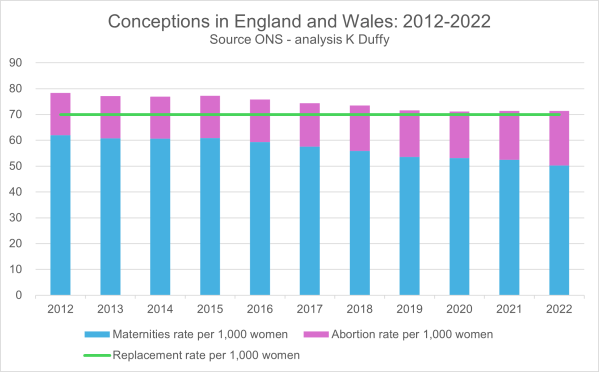
The numbers from the Office for National Statistics could not be clearer: England and Wales are falling short of replacement-level births, with maternities sliding year after year while abortions climb to nearly a third of all conceptions. On paper, the “missing” births are more than accounted for by abortions—but the idea that banning abortion could... Continue Reading →
In 2023, the NHS paid BPAS: £39,000,000 to provide abortions to women not using contraception, and £17,000,000 to provide abortions to women whose contraception had failed. It is hard to understand why BPAS is so enthusiastic about its campaign for improved contraception services across the NHS, including the morning-after pill, either it believes that effective... Continue Reading →
Are Gen Z aborting half of all pregnancies?
I was recently asked to verify my claim made in an earlier post that “half of all Generation Z pregnancies now end in abortion.” The most recent set of cohort fertility data was published by the Office for National Statistics in July 2025, showing conceptions, maternities, and abortions data for different age-groupings, over the years... Continue Reading →
“The government is fully aware of the numbers of women being admitted to hospital for treatment of abortion complications but for some reason seems unwilling to report these on an annual basis,” Duffy wrote. He called for greater transparency and accountability, arguing, “Deliberately minimising and misleading women about the reality of these risks is no... Continue Reading →
Grand Pinnacle Tribune
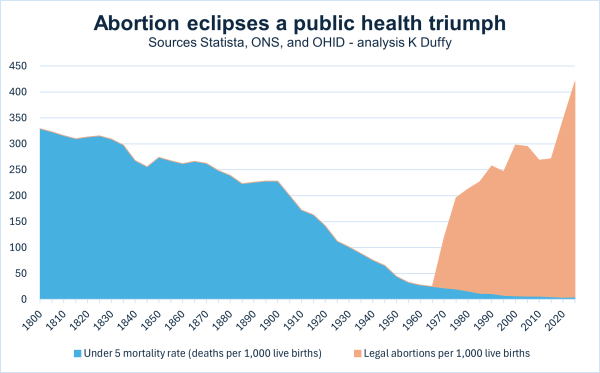
Abortion eclipses a public health triumph
In 1800, roughly one in three children died before their fifth birthday, reflecting an under-five mortality rate (U5MR) of 329 deaths per 1,000 live births. Faced with such high child mortality, women had just under six children on average to ensure that some survived to adulthood—a stark contrast to today’s average of just 1.45. Throughout... Continue Reading →
Grandparents are in decline
In August 2025, the Office for National Statistics published data showing the total fertility rate in England and Wales for 2024 was 1.41 children per women, the lowest value on record for the 3rd year in a row. There is little doubt that our birth rate is in decline—and so too are grandparents. The data... Continue Reading →
Duffy's NHS England analysis of hospitalizations for treatment of abortion complications, a rate of 1-in-17, reflects concerns raised by many in the United States regarding an increase in women visiting emergency departments after REMS safety regulations were weakened by the Food and Drug Administration (FDA) under the Biden-Harris administration. Biden's FDA also removed in-person dispensing... Continue Reading →
Live Action
Baroness Monckton of Dallington Forest, speaking during the Second Reading of the Crime and Policing Bill on 16 October 2025... Recent figures show that 54,000 women were admitted to NHS hospitals in England for the treatment of complications arising from the use of such abortion pills—a 50% rise from the figures before the pandemic. Analysis... Continue Reading →