An effective medical abortion is defined by the MARE Guidelines[i] as a successful expulsion of an intrauterine pregnancy without the need for surgical intervention, clarified by the following sub-categories:
- Continuing pregnancy: treated with surgical management
- Continuing pregnancy: patient opted to continue or outcome is unknown
- Retained products treated with surgical management (an evacuation of retained products of conception – ERPC)
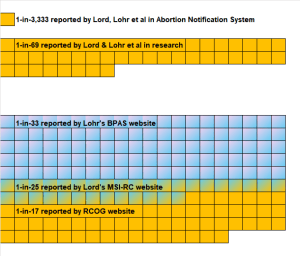
So, given the clarity of the above definition, why in the UK do we have official reporting of abortion complication rates ranging from a rare 1-in-3,333 to a common 1-in-17?
In 2021, Patricia Lohr and Jonathan Lord co-authored, with Aiken, a study into the effectiveness of early medical abortion in the UK.[ii] This study has since been widely cited and used by Lohr, Lord, and others in their campaigning for telemedicine abortion, otherwise known as pills-by-post or at-home abortion. The core claim in the study was that early medical abortion, whether performed in-clinic or at-home, is “safe and effective”. The results were used to persuade the UK Government to make telemedicine abortion permanent in August 2022, after the Covid-19 emergency measures were lifted.
The study used services data from BPAS, MSI-RC, and NUPAS for early medical abortions taking place in the first half of 2020. At this time, these three NHS-contracted independent organisations provided two-thirds of all abortions in England and Wales; Lohr and Lord, as the medical directors at BPAS and MSI-RC respectively, were accountable for the safety, quality, and reporting of more than 62% of the E&W total.
The Aiken study used the MARE guidelines and found 755 failed or incomplete abortions out of the 52,142 total sample; a complications rate of 1.4%, 1-in-69. To be clear, these 755 women required a surgical procedure, ERPC, to complete their abortion and remove any retained products of conception.
In the same year (2020), official reporting of abortion statistics by the DHSC and OHID indicated a complications rate for early medical abortion of just 0.03%, 1-in-3,333.[iii] This published rate used data submitted by the abortion providers in the HSA4 form and collated into the Abortion Notification System (ANS). As noted above, Lohr and Lord were accountable for about 60% of all data reported to the government. They knew from their own research and their own published data, that stating a complications rate of just 0.03% was disingenuous. So, how do we have this 48x difference in reported complications?
The ANS reporting by the abortion providers does not recognise nor report complications arising from a failed or incomplete abortion; this official reporting does not adhere to the MARE guidelines. The footnote on T8 of the ‘Abortion Statistics 2020:data tables’ states: “Total complications include: haemorrhage, uterine perforation, sepsis and/or cervical tear and are those reported up to the time of discharge. Therefore complications that occur after discharge may not be recorded.” [iv]
So, the ANS data do not include failed or incomplete abortions requiring a surgical intervention, and in any case are not a complete dataset.
In November 2023, the Office for Health Improvement & Disparities published what it refers to as a one-off report comparing complications data in the above-mentioned ANS and in the Hospital Episode Statistics (HES).[v] The latter is the system used by NHS hospitals to record and report cases of inpatient treatments. The HES data are for women who were admitted for the surgical treatment of complications arising from their abortion. Dr Jonathan Lord, as a consultant gynaecologist in the NHS, would be familiar with this inpatient ERPC treatment and the use of HES for recording such cases. The OHID report does not provide a breakdown of abortion method by gestational age, so we are unable to unpick just those complications arising from a failed or incomplete early medical abortion. That said, the report shows for 2020 (the same year as for Aiken and ANS above), an abortion complications rate of 1.76%, 1-in-57; it indicates a total of 3,695 complications arising from a total of 209,917 abortions across England and Wales. This is broadly aligned to the Aiken, Lohr, Lord et al findings, when extrapolated up to the total abortions in 2020, of 3,040 failed or incomplete early medical abortions requiring surgical intervention.
So what?
Complications arising from failed or incomplete medication abortions are easily identifiable, the inpatient treatment is well established, case data are known to the abortion providers, and the data are available for official reporting from HES. So why is the government saying that it will not make HES data a part of its annual reporting of abortion statistics? Continuing, as it has done so for 2022, to report just 300 abortion complications is very misleading.[vi]
As a first step, we should have annual reporting using the HES inpatient data. But that dataset will still be incomplete, we need to also know how many women are being treated as outpatients for abortion complications; typically using either expectant management or additional medication. The OHID says these cases are not recorded in HES, that other systems are used for outpatient departments such as A&E. The BPAS, MSI-RC, and Royal College of Obstetricians and Gynaecologists (RCOG) websites state medication abortion failure and incomplete rates of 3%, 4%, and 6% respectively.[vii] [viii] [ix]
Using as a proxy, Dr Jonathan Lord, with his many roles as an abortion provider and campaigner, we can see how confusing the abortion complications reporting landscape is:
- MSI-RC official ANS reporting to DHSC, approx. 0.03%
- BSACP research and campaigning, 1.4%
- NHS inpatient treatment, ERPC, recorded in HES, 1.76%
- MSI-RC public website, 4%
- RCOG public website, 6%
Surely, in the interests of full, honest disclosure and to ensure that women have access to reliable, accurate information before giving their informed consent, the government needs to fix this –
there is simply no excuse for continuing with complicated and incomplete reporting.
[i] Creinin, M. D., & Chen, M. J. (2016). Medical abortion reporting of efficacy: the MARE guidelines. Contraception, 94(2), 97–103. https://doi.org/10.1016/j.contraception.2016.04.013
[ii] Aiken, A., Lohr, P., Lord, J., Ghosh, N., & Starling, J. (2021). Effectiveness, safety and acceptability of no‐test medical abortion (termination of pregnancy) provided via telemedicine: a national cohort study. BJOG, 128(9), 1464–1474. https://doi.org/10.1111/1471-0528.16668
[iii] Office for Health Improvement and Disparities. (2024, May 23). Abortion statistics in England and Wales. GOV.UK. https://www.gov.uk/government/collections/abortion-statistics-for-england-and-wales
[iv] Abortion statistics for England and Wales: 2020. (2022, May 4). GOV.UK. https://www.gov.uk/government/statistics/abortion-statistics-for-england-and-wales-2020
[v] Complications from abortions in England, 2017 to 2021. (2023, November 23). GOV.UK. https://www.gov.uk/government/statistics/complications-from-abortions-in-england-2017-to-2021
[vi] Duffy, K. (2024, July 15). Complications from Medical Abortion are still being under-reported by the UK Government. Percuity. https://percuity.blog/2024/07/15/complications-from-medical-abortion-are-still-being-under-reported-by-the-uk-government/
[vii] BPAS. (n.d.). Abortion Pill | Treatment at home. https://www.bpas.org/abortion-care/abortion-treatments/the-abortion-pill/remote-treatment/
[viii] MSI Reproductive Choices UK. (2024, April 18). Frequently asked questions – MSI Reproductive Choices UK. https://www.msichoices.org.uk/support/frequently-asked-questions/what-are-the-possible-complications-and-risks-of-medical-abortion/
[ix] Abortion care | RCOG. (n.d.). RCOG. https://www.rcog.org.uk/for-the-public/browse-our-patient-information/abortion-care/
Discover more from Percuity
Subscribe to get the latest posts sent to your email.